Cutaneous Mass: A Case Report
 Saturday, July 13, 2013 at 12:07PM
Saturday, July 13, 2013 at 12:07PM Honorable Mention, Cases/Abstracts
Jacquelyn Horner, University of Georgia
1. Subjective:
Chance
4 YO male neutered boxer
Wt: 29 kg
Resides in Georgia
Chance is a blood donor for the UGA CVM Teaching Hospital. He undergoes yearly health screenings, which include physical examination, vaccination, and parasite testing. He is presenting today for his annual visit. He is bright, alert, and responsive. There are no abnormalities noted on physical exam, with the exception of a small, cutaneous mass on the lateral right hind leg. He has a BCS of 4/9. His lungs are clear and his heart is loud and strong. The owner states that the mass has been present for at least one year and has not changed in size during that time. It does not seem to bother Chance. The owner has noticed that upon manipulation, the mass undergoes temporary changes such as swelling and redness.
Chance was previously seen for routine bloodwork to be evaluated as a canine blood donor candidate approximately 6 months ago. A series of blood/diagnostic tests were run including: CBC, chemistry, urinalysis, tick panel, parasite smear, fecal flotation, heartworm test, and blood typing. There were no abnormalities found. The superficial mass was noted in the records at that time, but was not further evaluated.
Due to the patient history, breed, and physical exam findings, a fine needle aspirate was taken from the cutaneous mass.
Objective:
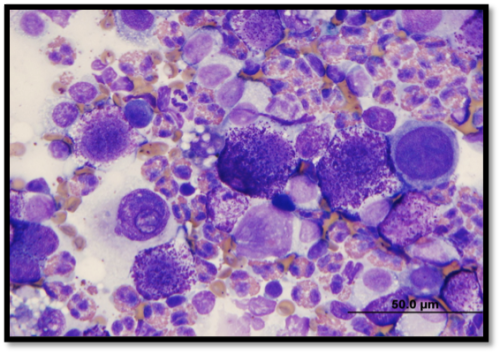
Chance has a cutaneous mass measuring 1cm X 1cm on his right lateral stifle. The fine needle aspirate cytology (Wright’s stain) revealed large numbers of round cells with purple intracytoplasmic granules:
Fine needle aspirate was attempted at the regional popliteal lymph node as well, but it was unsuccessful.
Assessment:
Presence of a proliferative population of round cells containing purple intracytoplasmic granules supports a tentative diagnosis of cutaneous mast cell tumor. It is important to note that Boxers are predisposed to this type of neoplasia. Due to the intermediate nature of differentiation seen on cytology and the unknown status of regional lymph node metastasis, this mast cell tumor is likely a grade I to II. Grade I tumors do not have regional lymph node involvement, contain well-differentiated cell populations, and are confined to the dermis. Grade II tumors have regional lymph node involvement with an intermediate level of differentiation, and extend to the dermis and subcutis. Grade II mast cell tumors are more likely to metastasize and cause systemic signs of disease. It is recommended to excise the mass with wide margins not only in hopes to prevent metastasis, but to also confirm diagnosis with biopsy and histopathology.
Plan:
Before surgery, blood and urine were collected for a full tick panel, CBC, blood smear, fecal flotation, and urinalysis as part of his annual exam and for pre-surgical health evaluation. Annual vaccinations were not given and were postponed to a later date.
Chance was sedated and placed under general anesthesia. A local block of the sciatic nerve was performed for optimal analgesia at the region of incision. The mast cell tumor was successfully removed with 1cm margins obtained and the deep facial plane resected. His incision was closed with little tension. Chance was recovered from surgery successfully and administered the following medications:
- Tramadol 50mg tabs – 2 tabs q8 hrs for pain control
- Carprofen 100mg tablet – ½ tab q12 hrs for pain and inflammation
- Famotidine or Pepcid – to prevent gastric ulceration/irritation
- Diphenhydramine or Benadryl – to suppress histamine release as a result of surgical manipulation
The excised mass was submitted for biopsy and histopathology. The results are attached and confirm the diagnosis of a Grade II cutaneous mast cell tumor.
2. Subjective:
Five days after surgery, Chance was taken off Carprofen. The next day, he developed pronounced pitting edema from the area of the stifle distally to the carpal pads.  The owner states that she immediately took him to her local veterinarian at home to obtain a prescription of Rimadyl to reduce the inflammation. Chance was also restarted on Famotidine and Diphenhydramine per counseling over the phone. Five days later, Chance presented to the Teaching Hospital for an irritated incision site, which the owner attributed to licking. He had otherwise been doing very well at home, with no changes in behavior or appetite, nor any coughing, sneezing, vomiting, or diarrhea.
The owner states that she immediately took him to her local veterinarian at home to obtain a prescription of Rimadyl to reduce the inflammation. Chance was also restarted on Famotidine and Diphenhydramine per counseling over the phone. Five days later, Chance presented to the Teaching Hospital for an irritated incision site, which the owner attributed to licking. He had otherwise been doing very well at home, with no changes in behavior or appetite, nor any coughing, sneezing, vomiting, or diarrhea.
Objective:
Chance has an incision of 6-7cm in length on his right lateral stifle. Upon physical examination, the incision site was mildly erythematous and swollen.
Assessment:
Chance was most likely licking the incision site, which caused mild trauma, irritation, and inflammation. Bacterial infection can occur if proper healing is not facilitated.
Plan:
Chance must wear an Elizabethan collar at all times to prevent further trauma and irritation to the surgical incision. He was prescribed the following medications:
- Carprofen 100mg tablet – ½ q12 hrs for inflammation and pain
- Cephalexin 250mg and 500mg tablets – 750mg q12 hrs for 10 days as prophylaxis for potential bacterial infection
- Famotidine – continued
- Diphenhydramine – continued
At home, the owner should monitor the incision for heat, swelling, discharge, malodor, or excess pain. Also, monitor for vomiting, diarrhea, or inappetance associated with reaction to the prescribed medications. She is advised to call the Teaching Hospital in the case of any of these observations. No running, jumping, or playing is permitted until sutures are removed in one week’s time, pending proper incision healing.
